This post was written for Escape Velocity Blog and first appeared there.
Since 2013, there has been an explosion of start-up activity in the Healthcare space in India. AngelList lists about 1,139 companies in the healthcare space in India. Fundamentally, the various activities that these start-ups are engaged in can be broadly bucketed into 9 spaces – locating and booking (doctor, pharmacy, diagnostic centres), telemedicine, managing health information, devices (fitness as well as medical), commerce, home care, practice management and networking / sharing within doctor communities, general information and content. Many companies are doing a mix of these activities.
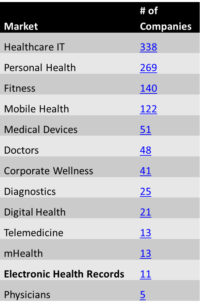
A quick dig into the data from AngelList in the table on the side; as it shows, much of the focus of entrepreneurial activity so far has been on connecting doctors and patients, and on digitising clinic / hospital operations. There are just 11 companies listed under Electronic Health Records and it is at the bottom of the list.
Why is management of health information / Electronic Health Records (EHR), languishing with just a few focusing on it?
What are EHR?
One generates so much health data without realising it; during any illness there’s the list of symptoms, medical history, diagnostic data (lab test, imaging…), treatment history (prescriptions and medications), progress notes etc., and even in the normal course of life there’s immunisation history (in the case of kids), allergies, biometric data (BP, sugar…), lifestyle choices (sleep, diet, exercise…) etc. These are all discretely recorded somewhere – on paper or as printed reports or as images or on wearable devices (including mobile phones!) – and then discarded later, except in the case of a chronic illness. Simply put, an EHR is a collection of all these medical records that are generated whenever an individual interacts with any healthcare service.
What are the advantages of systematically recording health?
Digitising health records has a host of rewards:
- Easy sharing of data with all stakeholders involved in patients care
- Better evidence based diagnosis and care as it provides a patient’s full history
- More accurate reporting by patients and faster diagnosis
- Better monitoring of medication or recommendation compliance / adherence
- Lower costs from reuse of old lab test results as well as from eliminating redundancies in data capture (and burden on office staff)
- Increases accountability of health care professionals
- Robust analytics including predictive analytics which can help governments make better health policy decisions or help insurers / medical product companies design and optimise their products better
In the case of India, recognising the importance of EHR to deliver Universal Health Coverage (UHC, ‘easily accessible and affordable health care to all Indians by 2020’), the High Level Expert Group (HLEG) constituted by the government recommended, ‘adoption of system-wide Electronic Medical Records’ (Recommendation 3.6.3).
So, coming back to the question, with so many advantages and a government push behind it, why are so few health start-ups working on EHR?
Who is generating the data and who’s digitising it?
Fundamentally, there are 3 places where this data is being generated – at the doctor, at the lab / pharmacy and by the user through devices. And there are multiple ways this data can be digitised – by any of the aforementioned or by an intermediary.
The best case to digitise information would be at the source – by the generators viz., the doctors or the hospitals. However, there are a number of reasons why this is not happening yet in India:
- Doctor’s maintain a record only when they see a long term need or opportunity. And, this need is felt only in some specialities where a patient can be retained longer or where the diseases are chronic. Some examples would be dentistry, gynaecology, psychiatry, paediatrics, diabetology and cardiology. Even in such cases, many a times, the physicians seldom take the responsibility for maintenance of records in any form. The general habit is to hand over the file to the patient who brings it for every consultation. Where the data is maintained by the physician, they use it to raise entry barriers and don’t give access even to the patient easily.
- In many other specialities, practitioners would argue that there is practically no reason to know a patients’ general history for certain illnesses. For example, in general medicine, most ailments are treated by assessing near term causes and not many doctors really bother about (or need to bother about) longitudinal health history before prescribing the next course of action. In many a case, history is disregarded as well and medical tests etc., are routinely redone though the previous ones are perfectly valid.
- Most of the current methods of digitising are cumbersome and demand extra time from the doctor. So these are not done in real time, passed on to low cost resources (usually interns and nurses) or are transcribed by an untrained third party later. Due to this, many a times, errors creep in; making the data unreliable and useless for future use.
- In spite of all these drawbacks, there is one place where massive health records are being generated at source – the hospitals – especially in the In-Patient Departments (IPDs). That’s because the rules under the Clinical Establishments Act were revised in 2012 , and then mandated ‘maintenance and provision of EMR/EHR for every patient’ for registration and continuation of all clinical establishments. However, most hospitals do it as a tick mark to meet compliance as data standards are still not in place (as of May’16, the Ministry of Health (MOHFW) was still seeking comments and views on the EHR standards from public). To meet compliance many small clinics and private hospitals scan and store hand written memos, and while many large private hospitals use EHR, they fail to deliver on the main criteria of standardisation and interoperability.
So, there are fundamentally two problems at source – behaviour change and lack of standards.
The second generator of massive amounts of health records are the numerous labs and pharmacies. And here is where the easy wins lie in digitising records but where there is little focus and attention from start-ups. Again, a host of factors stopping adoption:
- A lab is essentially a hotchpotch of instruments, each spewing data in its own proprietary format. The technicians then input them into the lab’s software which is mostly customised (a very fragmented custom software market exists in this space), which then gives out a report in a different format. The same is the case of pharmacies. A pharmacy can chose from hundreds of different software and enters data according to its own needs. One can enter the name of the medicine, test, doctor and patient in any way one desires. Lack of data standards, low integrity of master data.
- Each lab and pharmacy is an enterprise in itself. There are approximately 5.5 lac pharmaceutical retailers in India and organized retail contributes to less than 3% of total pharmacy retail sales. Many of them hand over handwritten bills or give out prescription medicines over the counter. Organised players control only 15-20% of diagnostics industry revenue. This fragmentation compounded by lack of digitisation and regulation amplifies the previous problem manifold and makes interoperability of data virtually impossible. Also, demand hugely outstrips supply so even these organised players don’t see any merits in long term engagement of captive and existing customer base.
So, again two big problems at the pharmacy or lab – lack of standards and regulation.
The third place where information digitisation can be done is through the user. This is what Google Health tried and what Microsoft HealthVault and some of the Indian health care start-ups are attempting. Users have to either manually enter health records, upload the data or authorise these companies to access their lab results, prescription history, and visit records from various partner labs, pharmacies, hospitals, and clinics. They can also connect their home-health devices and push data to a central repository. These companies would import, clean and merge potentially separate health records into one centralized health profile. Here again there are a host of barriers to digitisation:
- Many a times, the user doesn’t get electronic copies (especially of medical images which are difficult to scan). While one gets hard copies, manually entering information into a system is both painful and cumbersome. Even if one has the patience and enthusiasm to do it, errors happen due to limited understanding of the technical data being entered. And a big negative feedback loop is added, if doctors are not interested in looking at this data either due to habit or distrust of this data.
- One of the two reasons why a user would take the effort to organise and / or digitise his health history is the opportunity to use those for preventive care. However, prevention as a plank has seldom motivated Indian consumers to adopt something.
- Discerning consumers also might be concerned about confidentiality and security issues with data uploaded onto servers of relatively unknown third party players. Who will own data uploaded? Who all will access these records and for what purpose? These are all pertinent issues that the user has to be reassured about before uploading sensitive health data on the internet.
Though a company like Google tried this user driven approach to EHR to help one “make smarter choices”, it shut operations in 4 years.
Are there any successes? What are the reasons for the same?
There are some countries where information is digitised, of course, and a big part of it has to do with Government push both in terms of defining and enforcing standards and also forcing behaviour change via regulations.
In the UK, where health care services are free at the point of use to permanent residents via the NHS, it’s in the governments’ interest to set up the IT infrastructure to bring more efficiency and effectiveness into the delivery of healthcare. In the US, where insurance covers the high healthcare costs and pays the service provider directly, it’s in generators (doctors and hospitals) interest to maintain records in order. Then recently, Obamacare in USA both incentivised adoption at the beginning and penalised non-compliance later resulting in fast digitisation in Healthcare. That prescriptions are managed by a handful of third parties is also another big enabling factor.
Some home-health (especially fitness) device manufacturers have had limited success in terms of generating health information from users. Most of it has to do with real-time gathering of data, automation and gamification. But the data generated through these means is too trivial to be of use to impact healthcare in a significant way.
To summarise, digitising health care in India still remains a hard nut to crack under the existing circumstances – the size and complexity is just a small aspect, there are bigger behavioural and regulatory problems at play. Learnings from NHS and Obamacare show that a heavy external push from the government is required for entrepreneurs to focus on this area and succeed.
- With inputs from Arun Sahlam (Cofounder – HealthKonnect; Previous: Cofounder & CTO – CarWale)

